After 35 years as an oral surgeon, Dr. Arthur Wilk closed his practice in Clinton following “daunting challenges” caused by the COVID-19 pandemic. In Darien, Dr. Cecile Windels sold her pediatric practice to a hospital health system after enduring significant income losses.
They are among thousands of physicians and other health care professionals across the country who have made coronavirus-prompted career changes such as closing practices, joining larger health systems and retiring early. The reasons for the moves vary from declines in income due to fewer inpatient visits to increased operational costs for personal protective equipment (PPE) and fears of contracting the coronavirus known as SARS-CoV-2.
Health care advocates say the changes will exacerbate physician shortages, further erode the existence of private practices, decrease patient choice of doctors and obstruct continuity of patient care. A January report in Health Affairs, a peer-reviewed journal of health policy research, said: “Consolidation tends to lead to higher prices without strong evidence of quality improvements.”

Photo Courtesy of Dr. Windels.
Dr. Cecile Windels sold her medical practice in October to Stamford Health.
“The national trends are definitely happening in Connecticut,” said Dr. Gregory Shangold, president of the Connecticut State Medical Society. It will be more challenging for state residents to access high-quality care when physician shortages already exist, particularly in underserved, low-income areas, he said.
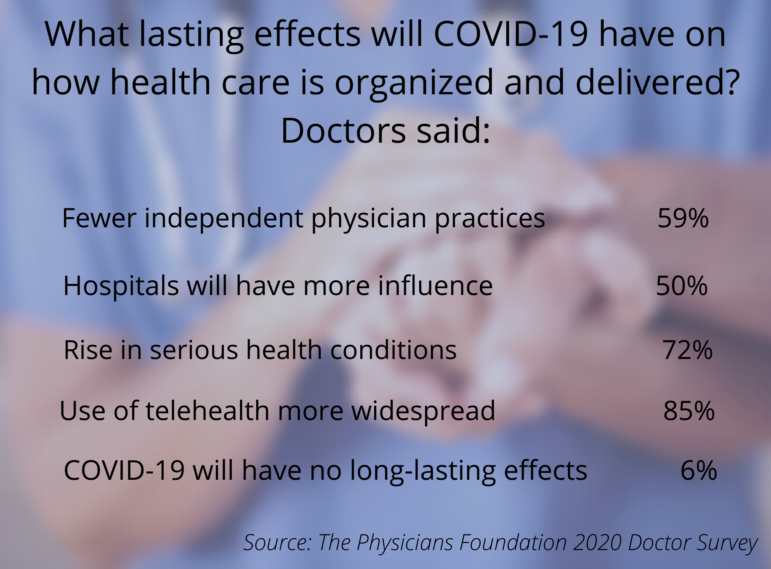
A national Physicians Foundation survey last July found that COVID-19 prompted the closing of more than 16,000 practices, 76% in private practice. The closings represented 8% of respondents. Another 8,000 closings were planned within a year. In addition, 72% of respondent doctors said their income dropped, 43% cut staff, and 16% had changed jobs or planned to within a year.
Ellen Andrews, executive director of the nonprofit Connecticut Health Policy Project, said fewer providers treating more people mean less time in a doctor’s office, higher prices and potential poor fits between patients and doctors because of such issues as language differences and transportation.
Andrews said that since mental health needs are skyrocketing during COVID-19, she is concerned about access to appropriate care. “With your surgeon, you don’t care if he’s a nice guy or not,” she said. “With mental health providers, you really do need a connection.”
Shangold heads a Willimantic-based emergency medicine practice that contracts with hospitals. He said he already sees people in emergency rooms for care typically provided by primary care doctors and specialists. “They can’t get one,” he said.
 Based on phone calls from physicians to the Fairfield County and Hartford County medical associations, there has been “a very definite uptick in the number of retirements and the number of physicians who have sold practices and work for someone else,” said Mark Thompson, their executive director. He said doctors have been seeking advice about how to close a practice and how to establish the monetary value of a practice. He would not provide statistics.
Based on phone calls from physicians to the Fairfield County and Hartford County medical associations, there has been “a very definite uptick in the number of retirements and the number of physicians who have sold practices and work for someone else,” said Mark Thompson, their executive director. He said doctors have been seeking advice about how to close a practice and how to establish the monetary value of a practice. He would not provide statistics.
In dentistry, the American Dental Association reported 72.7% of Connecticut dentists WITH lower patient volumes since the start of the pandemic, according to a survey conducted the week of Jan. 18. This was the fifth-highest in the country. Nationally, 56.2% of dentists reported lower patient visits.
Connecticut dentists considering selling or merging their practices will likely wait until after the pandemic because lower patient volume and reduced income hurt practices’ values, said Dr. Tam Le, president of the Connecticut State Dental Association.
For Wilk, who is 65, the pandemic struck from multiple fronts. His daughters said that they wouldn’t let him see his grandchildren if he kept seeing patients. Many patients didn’t want to go into the office. His surgical assistant couldn’t work because her child’s school closed. His other employee worried about contracting coronavirus.

Photo Courtesy of Dr. Wilk.
Dr. Arthur Wilk, an oral surgeon, closed his Clinton practice.
“Basically, we had a family meeting. It was mutually decided that it was not worth it,” Wilk said.
After closing in March, when elective surgeries were prohibited, Wilk reopened in June for patients who had been having ongoing treatment “to make sure they were squared away,” he said. He sent a letter to patients announcing his decision and made referrals to other surgeons.
Windels, the Darien pediatrician, said that when COVID-19 hit, her patient load dropped by 60%. She said finding available PPE was difficult, prices were astronomical, and other supplies, like strep and flu tests, were hard to get. She said she spent a lot of time on the phone answering parents’ questions about their children’s health, which she couldn’t charge for. She took a lower salary to avoid laying off staff.
A federal Paycheck Protection Program loan kept her afloat and prevented staff layoffs. “I would have had to close my door,” she said. She signed an agreement with Stamford Health Medical Group in October.
Windels still practices pediatrics in the office she has had since 2006. But now she is an employee of the health system, which handles the business side. “I don’t have to stay up at night worrying about my bills,” she said.
Dr. Rodrigo Acosta, president and chief executive officer of Stamford Health Medical Group, said he is in talks with two other medical practices to join the system. He also said that he has hired doctors who were laid off or had their salaries cut during the pandemic.
From 2016 to 2018, the number of Connecticut physicians affiliated with health systems grew in every part of the state, according to an analysis of “metropolitan statistical areas” by Health Affairs. For example, in the Bridgeport area, which includes Stamford and Norwalk, the number of doctors associated with the Yale New Haven Health System went from 33% to 42%. In the New Haven-Milford area, doctors associated with Yale New Haven rose from 29% to 43%. The national growth was the fastest in the Northeast and the Midwest.
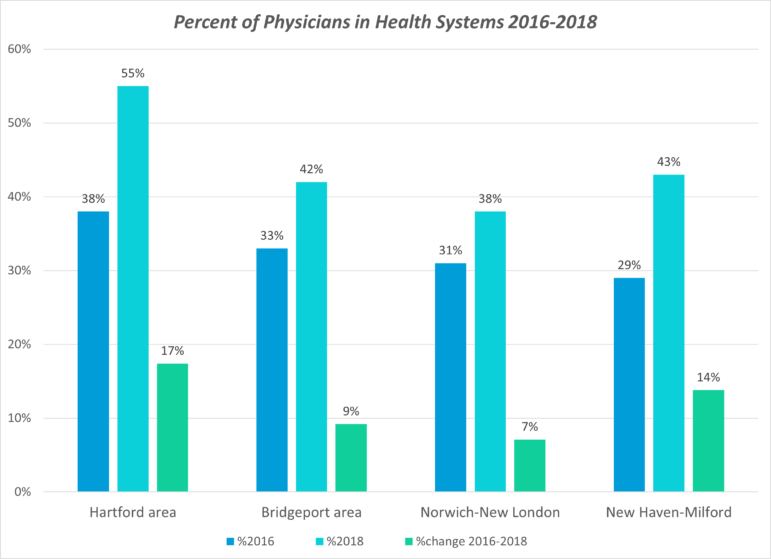
Graphic by Bonnie Phillips
Source: Health Affairs
Health systems benefit doctors by handling operating costs, negotiating with insurance companies for reimbursement, maintaining data for increased federal regulatory demands, and providing a regular paycheck.
Andrews said she has asked the General Assembly to establish a task force of independent experts to analyze the implications. “People do not understand how consolidation is impacting cost and consumer choice,” she said.
Wilk now works part-time at Yale New Haven Hospital, mainly supervising residents performing oral surgeries. He said the hospital could enact COVID-19 safety procedures that a small practice like his could not afford, such as more support staff, regular COVID-19 testing for patients, sufficient PPE, and a dedicated staff to clean and disinfect treatment areas after each patient.
Wilk said closing his practice ended relationships with long-time patients.
“That’s not the way you’d like to part with them,” he said.
Dr. Wilk is an outstanding oral surgeon, his need to close his practice is a real loss to the community.