The Westside Care Center in Manchester is ranked among the best nursing homes in Connecticut, receiving a ‘five-star’ rating for overall quality under a federal rating system.
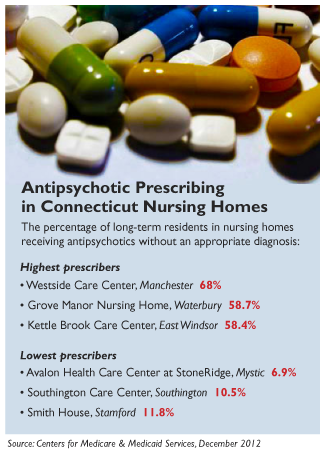
At the same time, Westside has the state’s highest percentage of residents who receive antipsychotic drugs, even though they do not have a psychosis or related condition that regulators say warrants their use. Federal data shows 68 percent of Westside long-stay residents were receiving the drugs – more than double the state’s average of 26 percent, which already ranks in the top-third of states nationally.
A C-HIT review of federal nursing home data from December found that Westside is not alone: High antipsychotic use, considered dangerous and unnecessary in many cases, does not impact quality ratings of nursing homes, and is often unknown to consumers selecting a home. In three-dozen Connecticut homes, at least a third of long-stay residents are on antipsychotics – yet nearly half of those homes have excellent overall ratings, of 4 to 5 stars. Only three have the lowest overall rating.
WebKazoo Graphic
In addition, the state Department of Public Health has rarely imposed more than minimal fines on nursing homes for excessive or inappropriate use of antipsychotics, inspection records show.
Antipsychotic drugs are an important treatment for patients with certain mental health conditions, such as schizophrenia. But the Food and Drug Administration has warned that the drugs have potentially fatal side effects, including the risk of infections and cardiovascular complications, when used in elderly patients with dementia. Still, nursing homes use the drugs “off-label” to calm patients who are agitated or confused.
Concerned about the drugs’ overuse, federal regulators last year announced a national initiative to slash their inappropriate use in nursing homes, saying that nearly 40 percent of residents with dementia were receiving the powerful sedatives even though they didn’t have a condition that would warrant it. A 2011 report by the US Inspector General found that 83 percent of Medicare claims for antipsychotic drugs for nursing home patients were off-label, or for unapproved conditions.
Connecticut ranked in the top four states nationally from 2005-10 in administering antipsychotics to residents without appropriate diagnoses, and was the highest or second-highest nationwide in antipsychotic use among high-risk residents, federal data shows.
Even with recent efforts to curb the drugs’ improper use, the state’s prevalence rate of unapproved antipsychotic use remains high – 25.7 percent of long-stay nursing home residents, which is higher than 34 other states. Tennessee has the highest rate, at 30.1 percent; Alaska has the lowest rate, at 12.7 percent. The national average is 23.8 percent.
In conjunction with the federal initiative, health care advocates in Connecticut have formed a coalition — coordinated by Qualidigm, a Medicare quality-improvement organization — to reduce antipsychotic use. The group is working to educate nursing home providers about the risks of using antipsychotics to treat dementia-related behaviors and to offer alternative interventions “instead of going straight to medications,” said Ann Spenard, vice president of program operations for Qualidigm.
Antipsychotics provide, at best, “minimal benefits” for behavioral and psychological symptoms of dementia, Spenard said. But in recent years, they have become a front-line treatment for agitation, aggression and other behaviors. Alternatives include consistent assignment of caregivers to patients, and behavioral interventions to eliminate anxiety “triggers” for residents, Spenard said.
“It’s a big change,” she said, noting that the drugs were widely marketed to elderly patients for dementia, despite FDA warnings. “It’s like trying to turn the Queen Mary. It’s not going to happen overnight.” But she added, “I believe the state of Connecticut will be successful” in reducing the prevalence rate.
Toby Edelman, senior policy attorney for the Center for Medicare Advocacy, said the federal government’s encouragement of alternative treatments for dementia is important, but tougher penalties for nursing homes that overuse the drugs also are needed.
“The other piece of this is stronger enforcement,” she said. “If they misuse the drugs and have to pay a $139 fine, what do they care? It’s the cost of doing business.”
A review of three years of online inspection reports shows the Connecticut Department of Public Health (DPH) routinely addresses findings that nursing homes have administered unnecessary drugs by imposing minimal fines. In only one case contained in online reports compiled by ProPublica did state inspectors characterize the violation as serious, defined as causing “harm,” and none of the violations was found to place residents in “immediate jeopardy,” the highest level of severity.
Nationally, citations against nursing homes for unnecessarily medicating patients are relatively rare: 1,213 instances in 2012, according to data from the Centers for Medicare & Medicaid Services (CMS). Of those, only 12 were classified as posing “immediate jeopardy.”
“Almost everything is considered ‘no harm,’” Edelman said. “How can improperly medicating someone, with all the risks involved, not be considered harmful?”
U.S. Health and Human Services Inspector General Daniel Levinson has proposed stronger state and federal penalties against homes that inappropriately use antipsychotics.
Wide Swings In Prevalence
The December data shows that more than half of Connecticut homes – 128 out of 233 — were dispensing antipsychotics without appropriate diagnoses at rates exceeding the national average. In addition to Westside Care Center, three homes had rates double the national average: Grove Manor Nursing Home in Waterbury (58.7 percent), Kettle Brook Care Center in East Windsor (58.4 percent), and Silver Springs Care Center in Meriden (55.4 percent). Westside, Kettle Brook and Silver Springs are all run by iCare management.
Only one in four Connecticut homes has an antipsychotic prevalence rate below 20.3 percent, the national goal proposed by CMS.
The rate of off-label prescribing swings widely – from the high of 68 percent, to a low of about 7 percent. The lowest prevalence rates as of December were at Avalon Health Care Center at Stonebridge in Mystic (6.9 percent) and Southington Care Center (10.5 percent).
Federal standards for medication safety in nursing homes are high. Regulations mandate that residents not be started on the drugs unless antipsychotic therapy is “necessary to treat a specific condition as diagnosed and documented in the clinical record.” For patients who do require antipsychotics, facilities must make gradual dose reductions and behavioral interventions in an effort to discontinue the drugs.
Administrators of nursing homes with high rates say that regulators’ rules governing the conditions warranting antipsychotics are too narrow, and that the drugs are sometimes needed to keep residents from harming themselves or others.
Janet Aliciene, administrator of Grove Manor, said the home’s off-label antipsychotic use is high because many residents have serious mental health problems. She said no resident is placed on an antipsychotic without an order from an advanced practice registered nurse, who talks with a physician.
“We do have higher numbers, but that’s because of our population,” she said.
Darryl LeCours, administrator of Westside Care, questioned the official CMS data, saying the nursing home’s “internal data reporting” showed off-label use of antipsychotics was about half of the prevalence reported by CMS, or 32.4 percent. He said the facility had significantly reduced off-label prescribing by “aggressive alternative treatments and collaboration” among medical, mental health and pharmacy staff. Also, he said, Westside residents have “a high prevalence of chronic mental illnesses.”
At Avalon Health Care, with the lowest prevalence rate in the state, staff members actively work to find alternatives for residents with behavioral problems, said Tina Lipp, the home’s MDS coordinator.
“We’re definitely not high on antipsychotics. We don’t like them,” she said. She said Avalon’s medical staff closely tracks residents’ behavior to identify and eliminate triggers that may set off agitation or depression and works to wean residents off the drugs.
Whether staffing levels are a factor in the use of sedating medications in nursing homes is a subject of debate. The Connecticut data indicates a correlation: 75 percent of the 61 homes with the lowest prevalence of antipsychotic use reported high staffing levels — 4 or 5 stars, under CMS’ five-star rating system.
Avalon and Southington Care both provided more hours of care per resident, per day, than the statewide average of 1 hour and 35 minutes of care by licensed nursing staff, and 2 hours and 27 minutes of care by certified nursing assistants (CNAs). Avalon reported 2 hours and 17 minutes of care by nurses, and 2 hours and 30 minutes of care by CNAs.
Spenard and Michelle Pandolfi, director of consulting services for Qualidigm, said there is no evidence of a direct link between staffing levels and use of antipsychotics.
“We don’t know. No one’s done that research,” Spenard said, adding that the key to effective alternatives is not just adding staff, but training them in interventions.
But Edelman said advocates believe that overmedication is “absolutely tied to insufficient staff. If there aren’t enough people, and there’s not consistent assignment, it’s much less likely that the staff are going to know the patient and know how to care for the patient. Instead, you get cases where a patient is agitated, and the nurse calls and says, ‘We need medication.’”
In some cases, nursing homes notify families when medications are added or changed; in others, families are not informed.
Paul Caron, a children’s mental health counselor, helped to form a “family council” at the New Haven nursing home where his mother and father were residents, out of frustration over a lack of information. When he learned that both of his parents were put on antidepressants, he said his questions about side effects were rebuffed. At one meeting, he said, a nursing home clinician told him, “If you have questions about the medications, you should look them up on the Internet.”
“If they don’t involve family members, they can’t get to know the patients – which is the one way they could reduce” the reliance on psychoactive drugs, he said.
Beyond The Stars
Despite the federal crackdown on off-label use, the antipsychotic rate is not factored into CMS’ complex five-star rating system, which ranks homes on indicators that include nine quality of care measures, as well as staffing levels and inspections. That means that homes with high levels of antipsychotic use may still receive high ratings on CMS’ Nursing Home Compare website, which offers information to consumers.
Twenty-five of the 36 Connecticut homes with the highest rates of antipsychotic use had high ratings on quality measures — four or five stars, signifying above-average care. Only two had the lowest rating of one star. The nine indicators used in the quality ratings include incidences of pressure sores and urinary tract infections, but not antipsychotics.
In Connecticut, as in other states, nursing homes cited for unnecessarily medicating patients or not properly monitoring antipsychotics usually face minimal fines. For example, the DPH cited Hamden Health Care Center in 2010 for failing to identify any behaviors that justified the use of antipsychotics for three residents, including one who was simply “mad at family” and “wanting to go home.” Similarly, last March, DPH inspectors cited Ledgecrest Health Care Center of Berlin for putting a resident on antipsychotics without proper justification and monitoring.
The two homes faced state fines of less than $750 each for violations including the medication lapses.
DPH spokesman William Gerrish said the agency is concerned about “the prevalence of antipsychotic medications administered to nursing home residents with no primary psychiatric diagnosis or related conditions” and supports CMS’ reduction initiative.
The DPH reviews medication use as part of its survey process, he said, and the state’s frequency of citing homes for lapses related to unnecessary drugs is higher than the regional or national averages. In addition to fines, the state requires homes to adopt corrective action plans when it finds deficiencies.
The DPH is actively participating in the Qualidigm-led coalition and sponsored a statewide training event in December that focused on initiatives to improve dementia care, Gerrish said. The coalition also is working with Connecticut’s long-term care ombudsman program to educate nursing-home resident advocates about proper medication use.
In September, U.S. Sen. Richard Blumenthal, D-Conn., and colleagues introduced a bill that aims to reduce off-label antipsychotic prescribing in nursing homes by requiring consent from family members, training staff in alternative treatments, and tightening reporting on the use of the drugs. Blumenthal called the excessive prescribing a form of “elder abuse.”
Nursing home advocates say the extensive use of antipsychotics for elderly patients was fueled by drug companies’ improper marketing of such off-label uses – a practice that the government has cracked down on in recent years.
To view nursing home ratings go to our data mine section or click here.
To hear WNPR’s report on this story click here.
It’s also fueled by the over-use of psych APRNs for every “behavior deviation” under the sun…
I was so pleased to find your article run full-page in my Sunday New Haven Register. My family was greatly affected by this harmful practice back in 2000. My aunt had lived for seven years in a CT skilled care facility. She suffered terribly and ultimately lost her life because of the long-term and sometimes off-label prescribing of multiple drugs. BIG PHARMA has a big presence here in our state. The pharmaceutical industry is a powerful influence in the FDA, in medical schools, in medical journals, in doctors’ offices, and direct-to-consumer ads. I am grateful to Sen. Grassley (though the newly released Sunshine Act disappoints), Pro Publica, the Furious Seasons blog and links, and No Free Lunch. Please continue to investigate and inform. Remind doctors of their oath, “First Due No Harm”. Urge patients and their families to ask about potential side effects, about comparison to placebo, about alternate forms of treatment. Urge them to check or ask about their doctor’s relationship with the drug manufacturer.
Pingback: Connecticut Center for Patient Safety, LLC | A Voice for the Health Care Consumer