Deaf residents report frequent issues with sign language interpretation at Connecticut hospitals and health care facilities, hindering their ability to understand medical care fully.
And though video remote interpreting (VRI) services are widely available at Connecticut hospitals, patients have reported mixed experiences with the technology.
The issues persist more than 30 years after passage of the Americans with Disabilities Act (ADA), which requires interpretation for patients and family members under the “effective communication” section of the law. In the last three years, the U.S. Attorney’s Office has negotiated four settlements with medical facilities in Connecticut for complaints related to communication with deaf patients.
“At one point, ADA and accessibility seemed to be very good,” said Marissa Rivera, an advocate with Disability Rights Connecticut (DRCT). “And now, in 2022, it has completely collapsed.”
The reasons are multiple and complex but often attributed to an ongoing interpreter shortage, which makes it hard to consistently secure in-person interpretation, especially during unplanned emergency room visits.
About 5% of the state’s adults have a hearing disability, a rate that jumps to almost 9% among people older than 60, according to U.S. Census figures. There are currently 497 registered interpreters in the state, though not all have the required certifications to work in medical settings.
C-HIT worked with The Daily Moth, a news organization that provides daily video news updates in American Sign Language, to provide an ASL summary of the story along with video interviews with some of the sources. Click play to see the story summarized by journalist Alex Abenchuchan.
Connecticut hospitals and state lawmakers have been meeting with advocates through a work group of the legislature’s Human Services Committee, which proposed a bill to accept additional interpreter certifications and better organize state services for the Deaf.
“I would say it’s a universal issue, meaning across the state, that we’re trying to address,” said Human Services Committee Chair Rep. Catherine Abercrombie, who serves Meriden and Berlin.
Deaf residents can file complaints with a hospital or through state and federal agencies, so it’s hard to get a complete picture of how many complaints have been filed. But DRCT gets weekly calls related to medical interpreting issues, Rivera said.
DRCT helped Mary Pat Donovan, 60, of Vernon, file a federal complaint after a mental health emergency in 2016 led to a three-day stay at Hartford Hospital’s Institute of Living. Donovan wasn’t provided an interpreter and therefore couldn’t participate in group therapy sessions or understand her care, according to her complaint, which was recently settled.
Donovan said the lack of communication during her stay made an already difficult situation harder and resulted in her getting the wrong medication.
“I felt like my self-esteem was kind of crushed,” Donovan said through an interpreter. “I wasn’t able to say what I wanted to say. I wasn’t able to express myself.”
Assistant U.S. Attorney William Brown, the civil rights coordinator for Connecticut whose office investigates complaints, said, “We want to work collaboratively with the hospitals. I would say, most of the time, they are responsive, and they want to do the right thing.”
“In the end, the goal is to make sure the Deaf community can communicate with their medical providers just like anyone else can,” said Brown.
Though video remote interpreting (VRI) systems are becoming more common and often touted for their quick access, they can leave patients stranded if technology issues occur.
“This sometimes comes down to life or death,” Rivera said. “We’ve had cases like that, where on someone’s deathbed, not having VRI working. It’s terrible.”
Sometimes, it may be hard to understand an interpreter through a screen in a medical situation, said Connecticut Association of the Deaf President Luisa Gasco-Soboleski.
“If I’m in pain or on deep medication, there’s no way that the video would work for me,” Gasco-Soboleski said through an interpreter. “It depends on the severity.”
Still, remote services might be the only option in some cases.
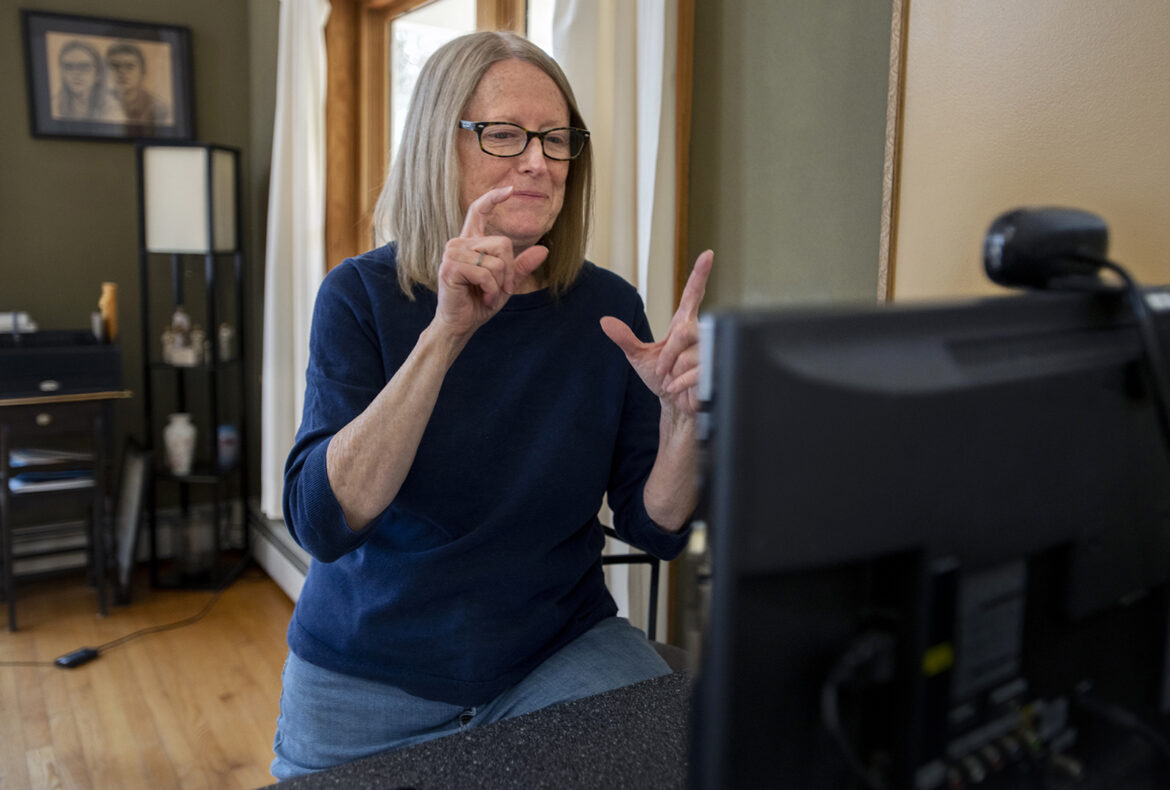
“On the one hand, people are saying we shouldn’t use VRI in the hospital because of the tech issues. But on the other hand, without VRI, we sometimes have no one,” said Doreen Simons, an American Sign Language (ASL) instructor at UConn. “I would rather have VRI than no interpreter.”
Simons has seen the issues from both sides: as a deaf patient and as a certified deaf interpreter helping other patients understand their care.
Simons of Farmington had emergency heart surgery at UConn Health Center in 2015. Her interpreter for the emergency room visit was having trouble hearing and couldn’t properly explain to her what was going on. When she woke up from quintuple bypass surgery, only her sister was available to interpret.

Melanie Stengel Photo.
Hospitals should provide interpreters for patients, Simons said.
“That was not appropriate at all,” Simons said through an interpreter. “They need to provide a certified interpreter. They should not be putting my family members in that situation.”
Her two adult children ended up interpreting several of the follow-up conversations with doctors after her surgery—emotionally processing the information while also serving in the official role of informing their mother.
Though Connecticut has been known as a leader in supporting deaf residents, advocates say services have declined in the last 10 years, contributing to problems in medical settings.
The state launched the Commission for the Deaf and Hearing Impaired in 1974, the first of its kind in the country. But in 2011, the commission was converted to an advisory council.
Amid budget cuts in 2016, the Department of Rehabilitation Services cut its sign language interpreting service. That same year, the state’s Office of Protection and Advocacy for Persons with Disabilities was eliminated, and tasks reassigned to Disability Rights Connecticut and the Department of Aging and Disability Services.
“We were the first in the country, and our services were awesome,” said Gasco-Soboleski. “And right now, we have zero. And I see more problems popping up, more problems appearing because there is no training.”
A 1998 Department of Justice consent decree, which required hospitals to provide an interpreter within an hour of notification for at least 80% of requests, expired. As part of the agreement, Connecticut Hospital Association contracted with sign language interpreters on behalf of all the hospitals. Without the decree in effect, advocates say compliance has lapsed.
A spokesperson for the Connecticut Hospital Association declined to be interviewed or answer specific questions through email but issued a statement noting hospitals’ dedication to patient care and work with advocates to address concerns.
Several hospitals, either proactively or as a result of complaints, are working on plans to improve services.
Stamford Hospital, for example, recently launched a long-term staff training on cultural considerations, working with interpreters, and basic sign language. The hospital has 30 video remote interpreting machines and a contract for translation services 24 hours a day in more than 200 languages, including ASL. It also has a contract for in-person interpretation and relies on 211 if no interpreter is available when needed.
“We have always had the standard of needing to provide appropriate interpretation services for patients,” said Liz Longmore, the senior vice president of ambulatory services and patient experience at Stamford Hospital. “It has become more of a challenge over time.”