I-Team In-Depth
Coronavirus Stresses Nursing Home Infection-Control Practices
|
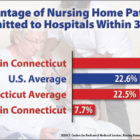
As coronavirus cases increase, posing heightened risks to the elderly, nursing homes will face growing scrutiny from state health inspectors. In Connecticut and nationally, complying with federal infection-control requirements is a challenge for some nursing homes. Between 2017 and 2019, 145 of Connecticut’s 217 nursing homes – or about 67 percent – were cited for infection-control violations, according to a Conn. Health I-Team analysis of data from the Centers for Medicare & Medicaid Services (CMS). (View list of nursing homes cited below).