Disparities
Years After Weight Loss Surgery, Patients Seek Treatment For Eating Disorders
|
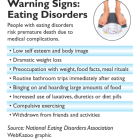
Morbidly obese individuals who had weight loss surgery are seeking treatment for eating disorders years after their procedure, prompting concerns among some experts about the assessment process used to identify surgical candidates. “They are terrified of gaining the weight back,” said Dr. Sara Niego, medical director of the Eating Disorders Program at Hartford Hospital’s Institute of Living, who has treated patients with anorexia, bulimia and binge eating disorder years after weight loss surgery. The lack of a national “gold standard” to psychologically assess prospective patients has led Connecticut mental health professionals to call for standardized criteria to identify those who are at risk before and after surgery. They worry some patients with mental health problems may slip through the cracks because each hospital and insurance company has different psychological screening requirements. “Unfortunately, there is no consensus in the field regarding what constitutes a psychological evaluation or what would prohibit an individual from obtaining surgery from a psychological standpoint,” said Kimberly Daniels, a clinical psychologist with the Center for Weight Loss Surgery at Middlesex Hospital.