Generation Health
Communication, Trust Needed To Reassure The Vaccine-Resistant
|
The Community Health Center Inc. set up shop inside the Boys and Girls Club of Greater Waterbury on a Friday in mid-July. Armed with 24 doses of the Pfizer COVID-19 vaccine, the team of six staff and volunteers sat ready for patients from 9 a.m. to 12 p.m.
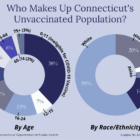
Not one person showed up. The turnout was not surprising, according to the vaccination site leader and nurses at the mobile clinic. Last month, new vaccinations across Connecticut fell to the lowest numbers since January, a predictable outcome when nearly 65% of the total state population has received at least one vaccine dose. But in Waterbury, only 46% of residents are fully vaccinated against the coronavirus.