I-Team In-Depth
State Restrains Psychiatric Patients At High Rate
|
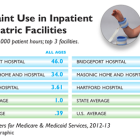
As the state works to improve its mental health system, new federal data show that hospitals in Connecticut restrain psychiatric patients at more than double the average national rate, with elderly patients facing restraint at a rate seven times the national average. In addition, the state lags behind in providing adequate post-discharge continuing care plans for psychiatric patients, especially teens and the elderly. Connecticut’s 28 inpatient psychiatric units and hospitals developed continuing-care plans for fewer than 70 percent of patients they discharged from October 2012 to March 2013 – indicating that thousands of patients may have left facilities without adequate treatment and medication plans. A C-HIT analysis of the federal data, released by the Centers for Medicare & Medicaid Services for the first time, show that Connecticut ranks in the top fourth of states (11th highest) in the use of physical restraints in inpatient psychiatric facilities – and is the third highest state in restraining patients 65 and older. Two psychiatric units – at Bridgeport Hospital and Masonicare Health Center in Wallingford – have the 10th and 12th highest rates of restraint use, respectively, among the 1,753 psychiatric facilities nationwide that are included in the federal reports, which cover October 2012 through March 2013.