Fines & Sanctions
Highest Prescribers Of Cancer Drug Paid As Speakers
|
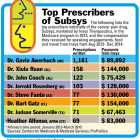
Eight of the top 10 prescribers of a potent narcotic used for cancer pain were paid more than $870,000 in speaking fees by the drug maker in 2013 and 2014 — indicating that Derby nurse Heather Alfonso was not the only high prescriber compensated by the company. Alfonso, an advanced practice registered nurse (APRN) who worked at the Comprehensive Pain and Headache Treatment Center in Derby, pleaded guilty last month to accepting $83,000 in kickbacks from 2013 to March 2015 from the drug company Insys Therapeutics, which has heavily marketed a painkiller called Subsys, a sublingual fentanyl spray approved only for cancer patients. Alfonso was paid to speak about Subsys at more than 70 “dinner programs,” but most of those programs were attended only by her and a sales representative for Insys, or by Alfonso’s colleagues and friends who had no authority to prescribe the drug, according to the U.S. Attorney’s Office for Connecticut. Alfonso faces a maximum prison term of five years and a fine of up to $250,000 on the charge of receiving kickbacks in connection with a federal healthcare program. In pleading guilty, she admitted that the money she was paid influenced her prescribing of Subsys, often to non-cancer patients, federal investigators said.