As cases of COVID-19 surged throughout Connecticut and the nation, “a perfect storm” of circumstances rendered nursing homes unable to handle the crisis, hastening the virus’ spread and deaths, experts say.
“It’s just kind of this perfect storm. It’s just the nature of the beast. This is the worst situation for a virus like this,” said Dr. David Hill, professor of medical science and director of global public health at Quinnipiac University Frank H. Netter MD School of Medicine.
Indeed, nursing homes care for an extremely frail population, many with underlying health conditions. The problems are compounded by staff shortages, lack of personal protective gear and proper staff training to care for residents in a pandemic. Even restricting visitors to emergency personnel only by mid-March could not stop COVID-19 from spreading rapidly among the state’s nursing home population.
On April 1, the state reported that 36 of the state’s 215 facilities had at least one confirmed case of COVID-19. On that date, there were 124 reported cases among nursing home residents and 13 had died. By April 17, the number of facilities with COVID-19 cases had tripled to 108, with 1,713 cases and 379 deaths. Those deaths represented 40% of the state’s COVID-19 deaths. But newspapers have reported higher death totals at some nursing homes.

Quinnipiac University School of Medicine Photo.
David Hill of the Frank H. Netter, MD School of Medicine at Quinnipiac University, said that there will be some silver linings through all the challenges facing nursing homes now.
Nursing homes, by and large, aren’t equipped to control communicable diseases quickly. Many have two-bed rooms, for instance, making it difficult to isolate residents who are ill. Often, staff members work more than one job, sometimes at multiple facilities, increasing the risk of staff contracting a disease and bringing it into a nursing home. The elderly tend not to exhibit typical symptoms of ailments; in particular, they’re less likely to have fevers than their younger counterparts, which can make COVID-19 more challenging to detect, Hill said. A lack of testing also is problematic.
“A nursing home right now is the worst place you can be during this pandemic,” said Dr. Richard Feifer, chief medical officer of Genesis HealthCare, which operates nursing homes nationwide, including 17 in Connecticut. “In many cases, it’s been impossible [to prevent the spread of the coronavirus], despite extensive measures.”
Connecticut nursing facilities have struggled with infection-control practices over the years. Of the 108 nursing homes with reported cases of COVID-19, 75 have been cited for infection-control violations previously (from 2017 to 2019), according to a C-HIT analysis of data from the Centers for Medicare and Medicaid Services (CMS).
Some facilities have been cited more than once, including RegalCare at New Haven, which has been cited four times; RegalCare at Southport, four; Whispering Pines of East Haven, three; and Salmon Brook Rehab and Nursing of Glastonbury, three. The violations include staff members failing to wash their hands, change gloves in between resident care or properly clean equipment after each use.
Staffing levels have been a mixed bag for the state’s nursing homes, CMS data show. Of the 108 facilities with COVID-19 cases, 25 have staff ratings below average or much below average. The remainder had ratings of average or above, data reported by Nursing Home Compare show. Even homes such as Caleb Hitchcock Health Center of Bloomfield, Edgehill Health Center of Stamford, and Nathaniel Witherell of Greenwich, with top 5-star ratings for overall performance and staffing, were not able to keep out COVID-19.
“The challenge with nursing homes is you have lots of very high-risk individuals together in close proximity with limited staff, staff that may not be salaried, and staff is caring for multiple patients,” Hill said. “This is kind of the perfect setting to spread a contagious organism.”
Nursing homes may have protocols for handling communicable diseases, Hill noted, but they’ve never experienced a pandemic like this, so “there probably aren’t robust, tried and true policies.” he said.
To help facilities with staffing needs, supplies of personal protection equipment and screening, the state has increased Medicaid reimbursements 15%, providing an additional $65 million. Also, the state will reimburse at $400 per day for COVID-positive residents in non-COVID recovery facilities. This rate is in effect for a maximum of 30 days per bed and will cost an estimated $15.4 million.
This week, the state announced that it will visit and inspect every nursing home in the state for infection-protection protocols. Also, CMS issued guidelines requiring nursing homes to report to CMS all virus infections and to notify residents and their families within 12 hours of a facility’s first positive COVID-19 test.
The state has partnered with Athena Health Care Systems to operate COVID-19 recovery centers for patients who are discharged from the hospital and need non-acute care.
The plan has its supporters and detractors, including some concerned about patient safety.
“I think that Connecticut is moving in the right direction by separating COVID-19-positive and negative individuals,” said Richard Mollot, policy researcher and executive director of the national Long Term Care Community Coalition in New York City. “However, this needs to be done thoughtfully, carefully, and with vigorous monitoring to ensure that it is done in the least harmful way possible.”
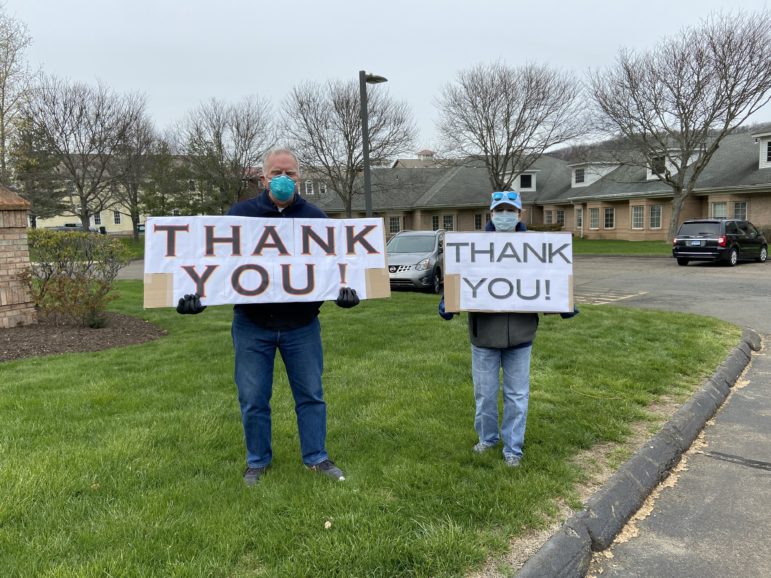
C-HIT.org Photo.
Two Woodbridge residents greet workers at The Willows nursing facility each day to show their appreciation. The facility is owned by Genesis HealthCare.
Lisa Freeman, executive director of the Connecticut Center for Patient Safety, said, “As a family member, I would be very concerned if my parent or spouse was moved to a location that I had little choice in, although it might be the best option. However, it seems clear that the safety of patients and staff, as well as providing the best environment for recovery and health, should drive the decision on this question.”
Mollot said, “It was probably never possible to protect residents 100%, but the slow and uneven pace of recognizing the obvious risk posed to residents undoubtedly resulted in unnecessary suffering and death. That being said, it is not too late to save many residents’ lives and families’ heartbreak.”
The weeks before Connecticut’s decision to lock down nursing homes, there was confusion and uncertainty nationwide about how fast the virus would spread, Hill said.
“I don’t think Connecticut took any longer time [to restrict visitors] than any other place,” Hill said, “and I think our governor has been really responsive all along the way during this outbreak.”
In hindsight, visitors should have been barred sooner, but that alone wouldn’t have curtailed the virus, Freeman said.
“Restricting visitors is one strategy, but without a comprehensive strategy, it is the equivalent of locking up a house and leaving the windows open,” she said. “The safety of residents was only as good as the weakest strategy for prevention of viral spread.”
Once the pandemic ends, nursing home leaders will be “looking at all the deficiencies that have been brought to light and starting to address them,” Hill said. Staff will be better trained in infection control, facilities will examine their ability to isolate residents, and protocols will be scrutinized, he predicted.
“There’s going to be so many things that get another look after COVID in the long-term care facility industry; it’s going to need an overhaul,” Hill said. “There will be some silver linings through all the challenges. There will be some positives.”
As the lessons from this pandemic—and the resiliency of the long-term care industry in general—unfold, nursing homes will look for ways to become more nimble when coping with a crisis, Feifer said.
“It really does become, in some ways, a resource issue. How well resourced is this industry?” he said. “This virus is unlike the world has ever seen before, and the next one, whenever that may be, will be different from this one too.”
Below is the state-issued list of nursing homes with cases of COVID-19 and deaths released on April 17. The nursing homes in red were cited for at least one infection-control violation between 2017-2019.
 Loading...
Loading...